Cancer treatment has witnessed a revolutionary shift over the past few decades—from conventional, broadly targeted methods to highly specific, immune-driven approaches. At the center of this transformation lies a promising class of drugs like ISB 2001, a trispecific antibody currently in clinical trials for relapsed/refractory multiple myeloma. Understanding how ISB 2001 works requires a brief journey through traditional cancer therapies, their limitations, and how immunotherapy is rewriting the rulebook of oncology.
Conventional Cancer Treatments: Power with Limitations
Historically, cancer has been treated using a combination of surgery, chemotherapy, radiation, hormone therapy, and more recently, targeted therapy. While these methods have saved countless lives, they are far from perfect.
- Surgery is effective for removing tumors that are localized, but it cannot address microscopic cancer cells or metastases.
- Chemotherapy uses cytotoxic drugs that kill rapidly dividing cells, but because it also harms healthy cells like those in the bone marrow, gut, and hair follicles, it results in serious side effects and immune suppression. Worse, cancer cells often develop drug resistance, making chemo less effective over time.
- Radiation therapy similarly damages DNA in cancer cells but often harms nearby healthy tissue and can, in some cases, lead to secondary cancers years later.
- Hormone therapy is used for hormone-driven cancers like breast or prostate cancer, yet it only works for cancers responsive to hormonal manipulation, and cancer often evolves to become hormone-independent.
- Targeted therapy—a more recent development—blocks specific genetic mutations or proteins (like EGFR or HER2) that drive cancer growth. But this method is only effective in patients whose tumors express those specific markers, and again, resistance often develops.
While these methods focus on attacking cancer directly, their biggest drawback is that they do not involve the immune system, nor do they train it to recognize and fight cancer long-term.
Enter Immunotherapy: Fighting Cancer from Within
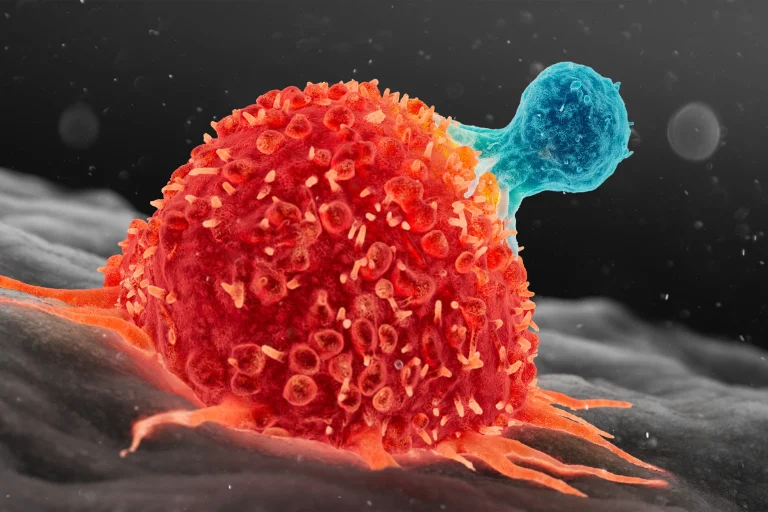
Unlike conventional therapies, immunotherapy activates the body’s own immune system to fight cancer. This approach is considered superior in many respects: it offers precision targeting, fewer long-term side effects, and most importantly, the potential for durable, long-lasting remission. Treatments like checkpoint inhibitors, CAR-T cell therapy, and bispecific or trispecific antibodies (like ISB 2001) have opened entirely new fronts in the battle against cancer.
ISB 2001, developed by Ichnos Glenmark Innovation, represents one of the most advanced forms of immune cell–redirecting therapy. It is a trispecific T-cell engager designed to simultaneously bind to CD3 (a receptor on T-cells), and to BCMA and CD38—two surface proteins commonly found on multiple myeloma cells. By doing this, ISB 2001 acts like a smart connector that brings the body’s immune soldiers (T-cells) into direct contact with the cancer, prompting the immune system to kill the tumor cells with precision. It is not preventive like vaccines against viruses, but rather therapeutic, given when cancer is already present and spreading.
Unlike a vaccine, which “trains” the immune system in advance of infection, ISB 2001 works in real-time, reprogramming immune cells to attack cancer immediately. While viral vaccines create long-term immune memory to prevent future infections, ISB 2001 acts more like a guided missile, linking immune cells directly to their target and unleashing their killing power right away. This mechanism holds particular promise in treating cancers that are resistant to conventional therapies.
A Growing Field of Global Innovation
ISB 2001 is not alone in this space. Global research groups such as Janssen (Johnson & Johnson), Gilead Sciences, Merus, Harpoon Therapeutics, and Hengrui Pharma (China) are all exploring trispecific or multispecific T-cell engagers that mimic or expand upon ISB 2001’s approach. Academic institutions like MD Anderson Cancer Center and research networks such as the Multiple Myeloma Research Consortium (MMRC) are also contributing to rapid advances in this field. These organizations are working to enhance the safety, potency, and flexibility of such therapies—making them more widely applicable across various cancers.
Conclusion: Toward Smarter, Safer Cancer Care
The development of ISB 2001 marks a pivotal point in cancer therapy—shifting focus from chemical or physical destruction of tumors to immune redirection and modulation. While conventional treatments will continue to play a role, their limitations—especially in advanced-stage or resistant cancers—make them less suited for long-term control or cure. Immunotherapies like ISB 2001 offer a targeted, durable, and potentially curative alternative. As research progresses and trispecific technologies mature, the future of cancer treatment may lie less in attacking cancer cells and more in empowering the body to do so itself.